Slow but Steady Progress on Palliative Care
Earlier this year, the Canadian Institute of Health Information (CIHI) released a report on access to palliative care in Canada. While caring for people at the end of their lives has always been important, the fact that people are living longer than ever has increased the general need for palliative care. Increasing access has become even more urgent with the legalization of medically assisted suicide in 2016 by Bill C-14, its expansion in 2021 through Bill C-7, and its further expansion to those with mental illness following the defeat of Bill C-314. Canadians need medical assistance in living rather than medical assistance in dying.
Why palliative care?
Palliative care is holistic, person-centered care for adults and children facing life-limiting or life-threatening illness. As our population ages and medical treatments improve, more Canadians live longer with life-limiting illnesses, and more die from chronic conditions than sudden causes like heart attack or accidents. Many people could benefit for years from the palliative approach to pain and symptom management.
Palliative care recognizes and respects inherent human dignity. It neither hastens death nor unnaturally prolongs life. It offers physical, emotional, spiritual, and social support to give patients their best possible quality of life despite illness or disability. It also encompasses the health and well-being of caregivers and family members.
Palliative care is team-based and involves a range of services delivered by a range of professionals – physicians, nurses, home care workers, pharmacists, physiotherapists, social workers, pastors, therapists, and volunteers may all have a role in supporting a patient and their family. Ideally, this support is available from diagnosis of a life-limiting illness through to natural death, is provided in a variety of settings, and extends into bereavement care for those left behind.
ARPA has covered the importance and need for palliative care in a 2017 Lighthouse News feature with Dr. Van Raalte, a 2017 documentary entitled “Ending Suffering: The Palliative Alternative,” and a 2021 policy report on palliative care.
Positive progress on access to palliative care
This CIHI report notes that some improvements have been made in Canada’s provision of palliative care in the past few years. For all deaths in home care, long-term care, complex continuing care and acute care, 58% of patients received some form of palliative care in 2021-22. This has increased from 52% five years earlier.
This public data from CIHI mirrors the data obtained by ARPA through an information request about the number of available palliative care beds in BC. This number has increased by almost 20% in a few short years.
Despite growth in the number of palliative care beds, the lack of growth of palliative care as a whole in the last two years might be indicative of the impact of the COVID pandemic and the allocation of health resources in other parts of the health system, a phenomenon that other provinces witnessed as well.
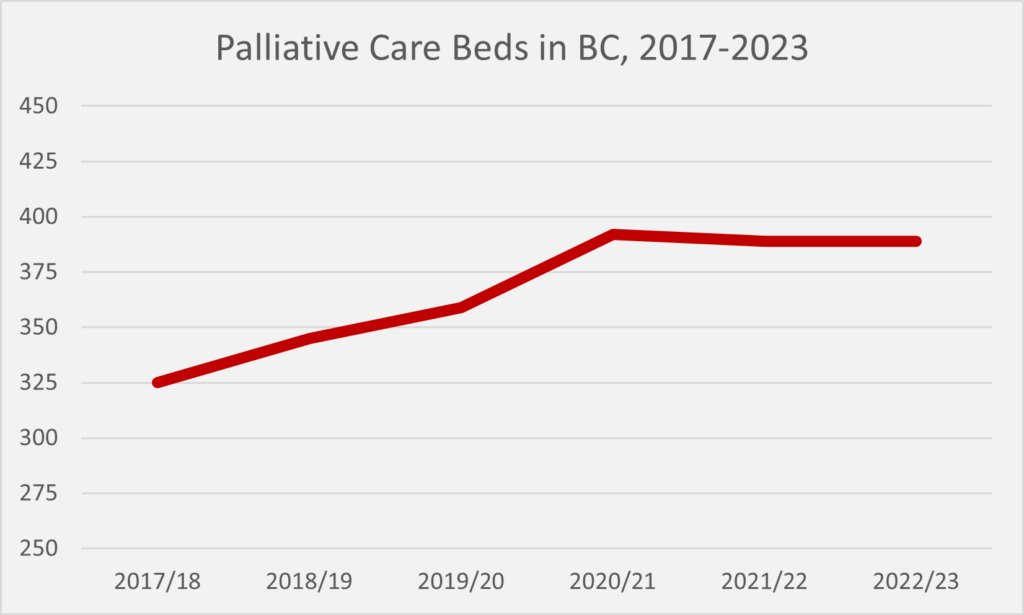
The number of palliative care bed available may seem low. Less than 400 palliative care beds in a province of over 5 million people? However, the average person admitted into a hospital palliative care bed stayed for only 12 days before either passing away at the hospital or being discharged. Thus, the average palliative care bed in a hospital will support 30 patients over the course of the year.
Unfortunately, Canadians who are requesting medically assisted suicide are not receiving palliative care at any significantly higher rate than those who are not suicidal, despite the fact that they stand in the greatest need of care. While 52% of all patients received palliative care before they passed away in 2016-17, only 59% of patients who requested medically assisted suicide received palliative care in any setting. Less than half of patients requesting assisted suicide had a member of a palliative care team weigh in on this request.
Most Canadians, given the choice, prefer to die at home instead of in a hospital. Providing palliative care at home makes passing away as comfortable as possible. Canada has certainly gotten better at providing more palliative care at home during someone’s final days. Thirteen percent of Canadians who died in a health care setting died at home with palliative home care in 2021-22. That is almost twice as many as five years ago. However, Ontario is responsible for almost all of this change, with 18% of those who died receiving palliative care at home. Provinces like Alberta (6%) and British Columbia (2%) need much greater investments in palliative home care, especially when British Columbia has the highest percentage of people dying by medically assisted suicide (4.8% of all deaths).
More progress is needed
Canada needs better data on palliative care. Due to data limitations, this CIHI report could only report on Ontario, Alberta, British Columbia, and Yukon. More provinces and territories need to track palliative care so that we understand the full need for palliative care in Canada.
Canada also needs better standards of palliative care. Although we know how many people accessed some sort of palliative care (in four of Canada’s provinces/territories), we still do not know the quality of this palliative care. Did the palliative care adequately control pain? How cost effective is home-based versus hospital-based palliative care? How well are patients and caregivers satisfied with the palliative care provided? We do not know the answers to those questions.
And finally, Canadians still need better access to palliative care, especially those actively considering assisted suicide. In their survey of palliative care five years ago, CIHI reported that up to 92% of Canadians could benefit from palliative care some time in their life. The fact that only 58% of Canadians who died in a health care setting (e.g. a hospital, hospice, or home care) obtained any sort of palliative care suggests that many more Canadians stand in need of palliative care. We continue to need more investments and more education around palliative care in Canada so that people at the end of their lives are properly cared for rather than offered and given assisted suicide.